Abstract
Background
A recent study found that approximately one of every six patients hospitalized for the first episode of syncope had underlying pulmonary embolism (PE). As current guidelines do not strongly emphasize on evaluation for PE in the work up of syncope, we hypothesize that there might be a higher rate of 30-day readmission due to untreated venous thromboembolism (VTE). The objective of this study is to measure 30-day readmission rate due to VTE and identify predictors of 30-day readmission with VTE among syncope patients.
Methods
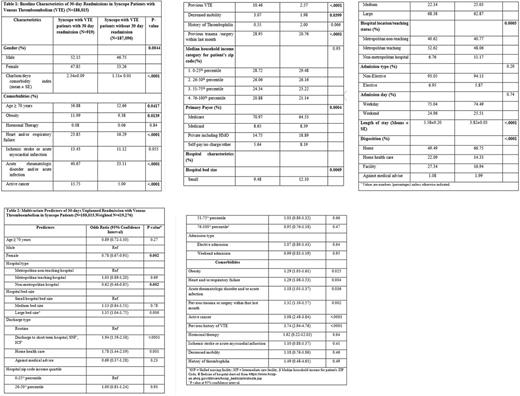
We identified patients admitted with syncope with ICD9 diagnoses code 780.2 in the Nationwide Readmission Database (NRD-2013), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality. The 30-day readmission rate was calculated using methods described by HCUP. Logistic regression was used to identify predictors of 30-day readmission with VTE. Discharge weights provided by HCUP were used to generate national estimates.
Results
In 2013, NRD included 207,339 eligible patients admitted with syncope. The prevalence rates of PE and DVT were 1.1% and 1.4%, respectively. At least one syncope associated condition was present in 60.9% of the patients. Among the patients who were not diagnosed with VTE during index admission for syncope (N=188,015), 30-day readmission rate with VTE was 0.5% (0.2% with PE and 0.4% with DVT).
Conclusion
The prevalence of PE in syncope patients was low in our study compared to the recently published report. Moreover, the 30 day readmission rate with VTE was also significantly low in patients with and without syncope associated diagnoses during index admission. Extremely low 30-day readmission rate with VTE argues against missed diagnoses of VTE in index admission for syncope. These results warrant a prospective investigation about the clinical impact of aggressive work up for PE in patients admitted with syncope without associated risk factors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal